The latest on everyone’s mind is the Zika virus. Zika is named for the forest in Uganda where it was identified in 1947. Generally, Zika is not serious–80% of infected people have no symptoms; most who become ill only develop nonspecific fever, rash, joint aches and red eyes lasting under 1 week. Rarely, it has been associated with, (not proved a cause of) a serious neurologic condition called guillain-barre syndrome.
In the last year Zika has spread rapidly through the Americas. No one knows exactly why this happened, but it had not previously been known in this part of the world and encountered a large “infection naive” population. Those circumstances can frequently result in this type of infection spread pattern. Zika spreads with a bite from infected aedes mosquitoes. 3 points about aedes: in warm weather aedes mosquitoes have been spotted as far north as Washington DC and possibly central NJ, aedes also harbors dengue and chikungunya virus, and climate change will likely cause aedes’ habitat to expand. There are unconfirmed reports of Zika spread via sexual contact.
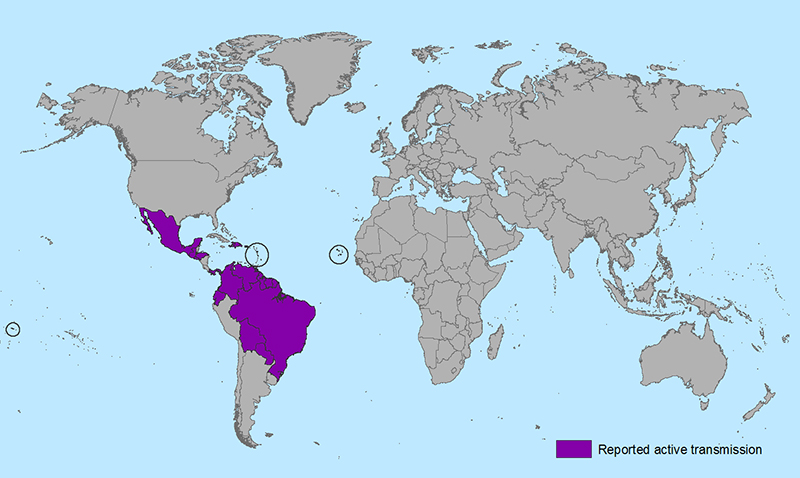
The above map from the CDC shows the spread of Zika in the Western Hemisphere. The epicenter is in Brazil (note: 2016Summer Olympics in Rio de Janeiro) but it has been identified as far south as Uruguay and has moved north inexorably through the Caribbean, Central America and Mexico.
Note this map of aedes mosquito locations:
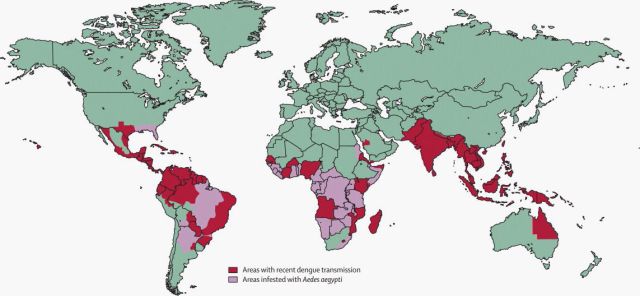
The above from The Lancet shows aedes in sub-Saharan Africa, south Asia, the South Pacific and parts of Australia, and most importantly for us Americans the US Gulf Coast and Hawaii.
The danger from Zika is to the unborn baby via maternal infection. There is strong association with, but again no positive diagnostic proof of, Zika and poor fetal brain development leading to microcephaly (small, abnormally shaped skull) and brain calcifications. Therefore, the center for Disease Control has issued several guidelines for women who are or may become pregnant (as 50% of all pregnancies are unplanned, these recommendations should be considered for all women of child bearing years):
- Consider postponing travel to areas with Zika outbreak.
- If traveling to those areas, as much as possible wear long sleeves and pants (preferably with insect repellent chemicals) and sleep in air conditioned rooms or under insect repellent netting.
- It is not recommended that all pregnant women traveling to those areas be tested for Zika, only for those coming from infected areas who develop fever, rash, red eyes, and joint pains.
- Women coming from Zika infected areas should have serial ultrasounds to evaluate for microcephaly and cerebral calcifications.
- Women who may be carrying fetuses suspected with microcephaly or cerebral calcifications should be tested for Zika.
- Women found to be Zika infected should be tested for dengue and chikungunya.
I am no alarmist but this is certainly a concern. It is spreading rapidly and no one knows where the limit may be. Still, if we follow the above and keep our wits about us there’s no reason to panic.
Questions? Comments? Thanks for following.




